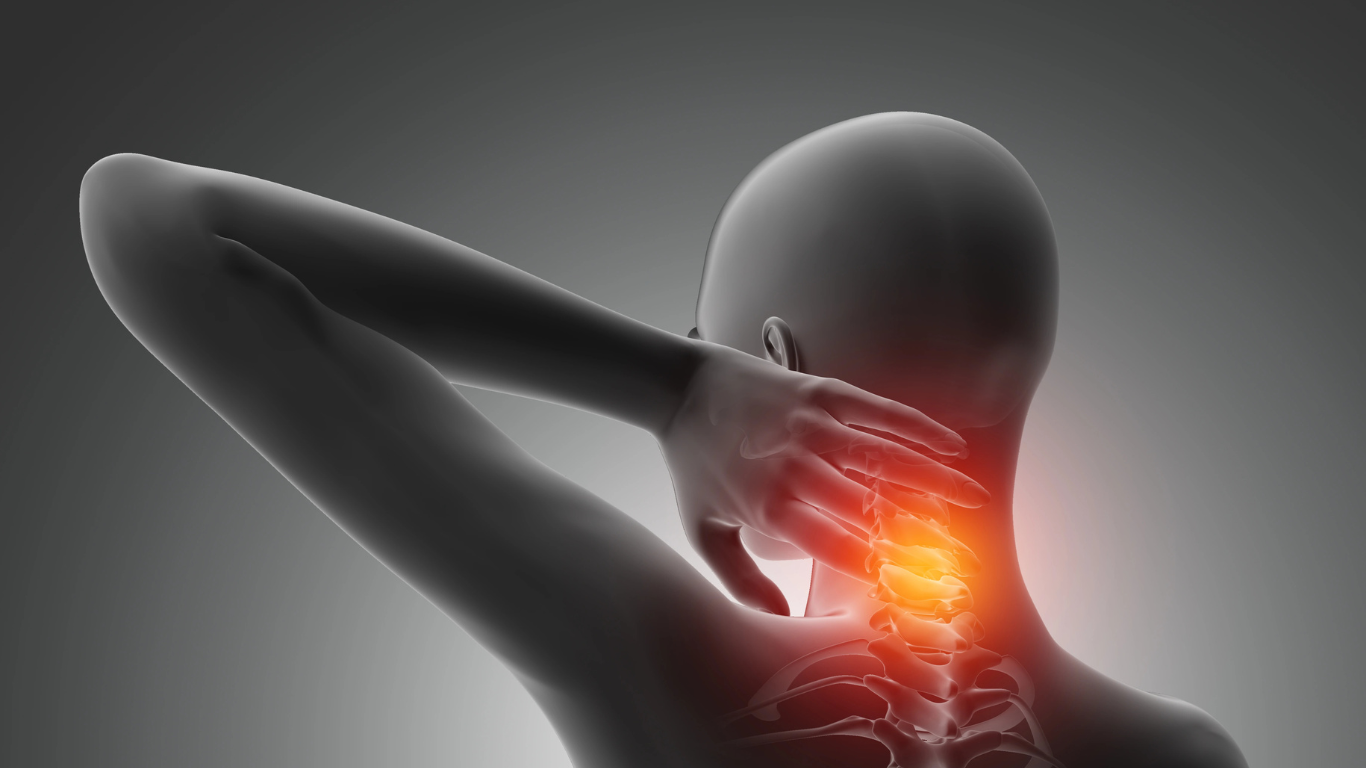
Cervical spondylitis, a degenerative condition affecting the cervical spine, is becoming increasingly prevalent in today's fast-paced, technology-driven world.
As more individuals find themselves hunched over screens for extended periods, the risk for this condition rises.

What Causes Cervical Spondylitis and Risk Factors to Consider
Several risk factors can predispose individuals to the development of Cervical Spondylitis. One of the more uncontrollable risks is a family history of neck pain or degenerative spinal conditions, which suggests a genetic component to the disease. Additionally, lifestyle choices, such as smoking and obesity, exacerbate the likelihood of developing spinal degeneration due to inadequate nutrition and increased stress on the vertebral structures. People who engage in heavy lifting or repetitive neck movements as part of their occupation may also be at higher risk due to prolonged strain on the cervical region.
In addition to these intrinsic factors, certain medical conditions may contribute to the development of Cervical Spondylitis. For instance, individuals with rheumatoid arthritis, diabetes, or other systemic diseases might experience accelerated degeneration of the cervical spine. Furthermore, injuries sustained from accidents or sports can lead to accelerated wear of cervical components, increasing susceptibility to spondylitis. Awareness of these risk factors is crucial; early intervention can often mitigate the progress of the condition and improve overall quality of life.
Ultimately, understanding what causes Cervical Spondylitis and recognizing the associated risk factors can empower individuals to adopt preventive measures. Engaging in regular exercise, maintaining a healthy weight, and practicing good posture are essential strategies that can help reduce the likelihood of developing this condition. Regular check-ups with healthcare providers can also facilitate early detection and the implementation of effective management strategies, ensuring that those affected can lead active, pain-free lives.
Diagnosis and Tests for Cervical Spondylitis
To further investigate the presence and extent of Cervical Spondylitis, several imaging tests may be utilized. X-rays are often the first line of imaging, allowing doctors to visualize bone changes such as osteophyte formation and any degeneration of the discs and vertebrae. However, for a more detailed view, magnetic resonance imaging (MRI) is frequently employed, as it can reveal soft tissue structures, including intervertebral discs and nerve roots. Additionally, computed tomography (CT) scans might be used in certain cases to provide precise anatomical details, particularly if surgery is being considered as a treatment option.
In some scenarios, additional diagnostic tests may be warranted to rule out other conditions or to further assess neurological function. Electromyography (EMG) and nerve conduction studies can help evaluate nerve compression or damage associated with Cervical Spondylitis. These tests assess the electrical activity of muscles and the speed of nerve impulses, providing insight into how well nerves are functioning. Ultimately, a combination of clinical evaluation and these diagnostic tests allows healthcare providers to develop tailored treatment plans aimed at alleviating symptoms and improving quality of life for patients dealing with Cervical Spondylitis.
Physical Therapy and Exercises for Cervical Spondylitis
A tailored physical therapy program for Cervical Spondylitis typically begins with an assessment by a qualified therapist, who designs a regimen suited to an individual’s unique needs. Initial sessions may focus on gentle stretching exercises that help restore range of motion in the neck. Techniques such as chin tucks and neck rotations can be effective in easing stiffness and enhancing mobility. Alongside stretching, strengthening exercises targeting the neck and upper back muscles are crucial. By reinforcing these areas, patients can better support the cervical spine, potentially reducing the recurring cycle of pain and discomfort.

In addition to these exercises, physical therapists may also incorporate modalities such as heat, ice, or electrical stimulation to help manage pain symptoms. Education plays a vital role in the therapeutic process as well; patients are often instructed in proper posture habits and ergonomic adjustments in their daily activities. By addressing lifestyle factors, individuals dealing with Cervical Spondylitis can help mitigate future flare-ups and maintain their progress in physical therapy.
Surgical Options for Severe Cases of Cervical Spondylitis
One of the most common surgical procedures for severe cervical spondylitis is anterior cervical discectomy and fusion (ACDF). This procedure involves removing the damaged disc that is causing compression on the spinal cord or nerve roots, followed by fusing the adjacent vertebrae to stabilize the spine. The goal is to alleviate pressure, improve pain symptoms, and restore function

For those with multi-level cervical spondylitis or where the traditional ACDF is not suitable, posterior cervical decompression may be an option. This surgical approach focuses on removing bony growths or other structures that compress the spinal cord or nerves from the back of the spine. In some instances, this may be combined with a fusion or instrumentation to enhance spinal stability. Each surgical intervention is tailored to the specific needs of the patient, based on factors such as the degree of spinal cord compression, age, overall health, and the presence of other spinal disorders.
Therefore, a thorough discussion with a healthcare provider is crucial to weigh the benefits and risks involved. With advancements in surgical techniques and technology, many patients can experience significant improvements in their symptoms and overall quality of life, paving the way for a return to daily activities and a more fulfilling lifestyle.
Lifestyle Changes to Help Manage Cervical Spondylitis
Diet also plays a pivotal role in managing Cervical Spondylitis. A balanced diet rich in anti-inflammatory foods—such as fruits, vegetables, whole grains, and healthy fats—can help reduce inflammation in the body, which may alleviate some discomfort associated with the condition. Staying well-hydrated is equally important; adequate water intake helps maintain spinal health and joint integrity. Additionally, being mindful of body weight can help lessen the load on the spine, further reducing the risk of exacerbating symptoms.
Lastly, stress management techniques such as meditation, mindfulness, and deep breathing exercises can provide significant relief from pain associated with Cervical Spondylitis. Stress often contributes to muscle tension, particularly in the neck and shoulders, so finding effective ways to unwind can enhance both mental and physical health. By implementing these lifestyle changes, individuals can take proactive steps toward managing their condition, improving their quality of life, and enjoying a more active, fulfilling existence.
Preventing and Coping with Cervical Spondylitis: Tips and Strategies
Regular physical activity plays a crucial role in preventing Cervical Spondylitis. Engaging in exercises that strengthen the neck and shoulders helps build resilience against degeneration. Activities such as yoga and swimming promote flexibility and support overall spinal health. Incorporating specific neck stretches into your daily routine can also provide relief and enhance mobility. It's essential to listen to your body and avoid activities that exacerbate pain, as overexertion can lead to further complications.
For those already experiencing the symptoms of Cervical Spondylitis, seeking professional help is vital. A physical therapist can design a personalized exercise program to strengthen the neck and back muscles while ensuring proper alignment. Additionally, alternative therapies such as chiropractic adjustments, massage, or acupuncture may provide symptomatic relief. Prioritizing self-care, making informed lifestyle choices, and actively engaging in preventive strategies are key steps in coping with Cervical Spondylitis and maintaining a healthy, active life.











Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.